As part of the ongoing support for the Chronic Condition Management (CCM) changes introduced from 1 July 2025, Bp Premier version Spectra SP1 Revision 3 delivered new claiming logic to improve the handling of relevant MBS item numbers across the finalise visit and invoicing workflows.
Finalise Visit MBS Item Enhancements
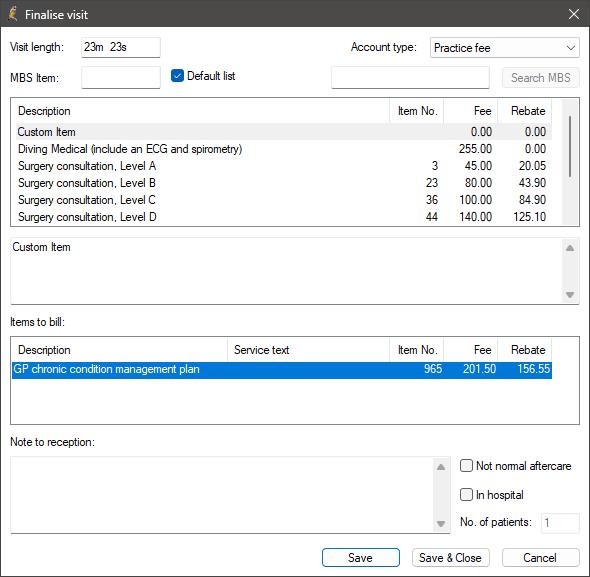
From Spectra Revision 3 and later, Bp Premier will now suggest appropriate item numbers when a user finalises a visit involving the preparation or review of a chronic condition care plan. Bp Premier will determine the correct item based on provider type (VR or Non-VR) and visit mode (face-to-face or telehealth):
Vocationally Registered (VR) GPs:
- Face-to-face: 965 (creation), 967 (review)
- Telehealth: 92029 (creation), 92030 (review)
Non-Vocationally Registered (Non-VR) GPs:
- Face-to-face: 392 (creation), 393 (review)
- Telehealth: 92060 (creation), 92061 (review)
The appropriate MBS item number will be displayed in the item picker based on these criteria.
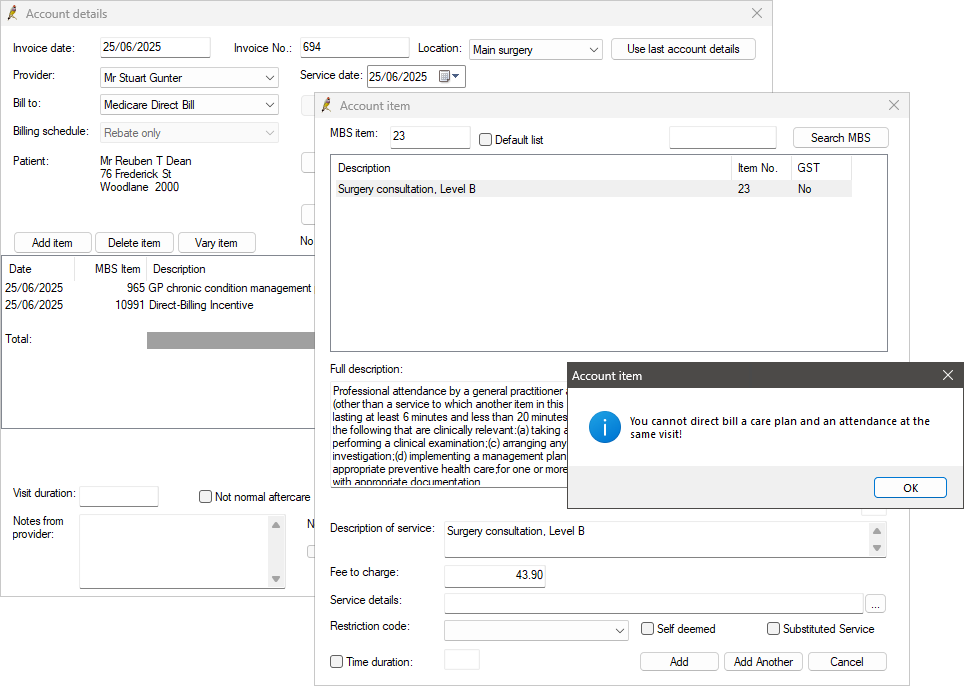
Co-claiming logic
In Spectra SP1 Revision 3 and later, Bp Premier now enforces co-claiming restrictions when CCM items are added during the finalise visit or invoicing workflows. These restrictions reflect current Medicare billing rules and are supported by system prompts where applicable.
The following co-claiming rules are applied:
- 965 / 392 and 92029/92060 (telehealth creation) cannot be billed with any other attendance item number.
- 967/393 and 92030/92061 (telehealth review) cannot be billed within a 3-month period unless there are extenuating circumstances.
Frequently Asked Questions
How do the Item number suggestions work for reviews?
Suggested item numbers for care plan reviews are date dependant and can be performed after 3 months if clinically appropriate. From the clinical record, if the provider tries to add a new care plan after 3 months, the system will prompt the provider to review the plan.
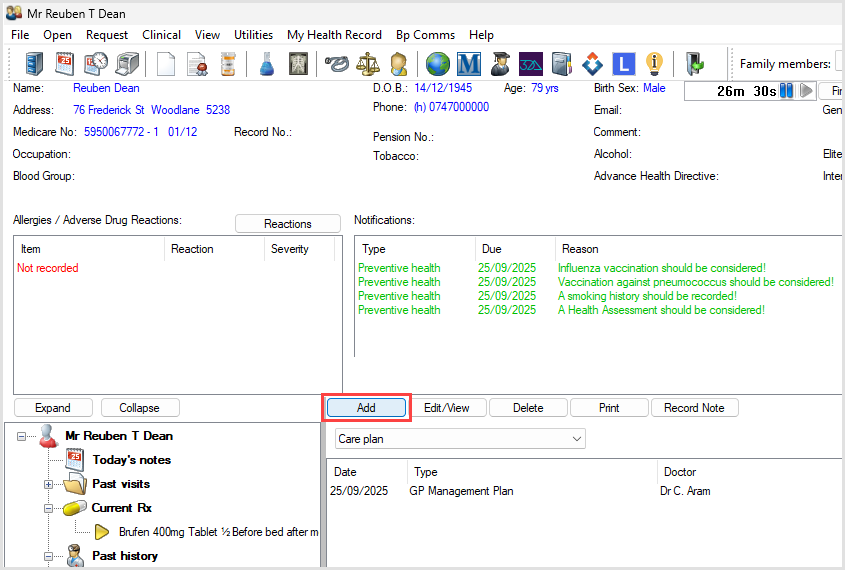
If you select 'Yes' from the prompt, a care plan review will be created. Appropriate item numbers for review of care plans will be suggested when finalising the visit for billing:
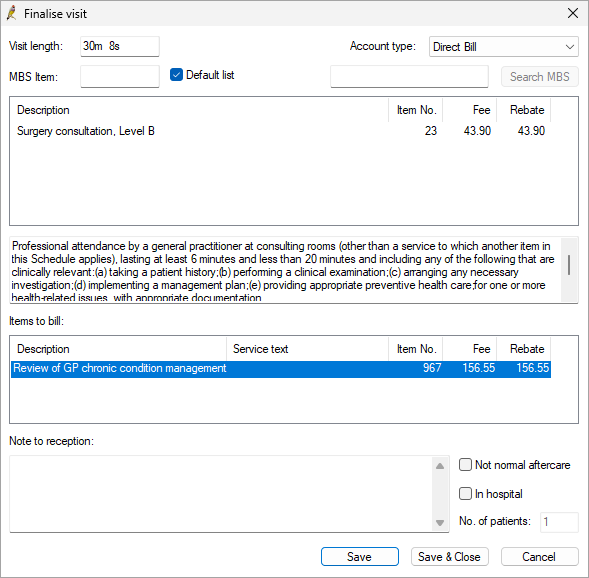
If the appointment type and the visit type is telehealth or telephone, then review item number 92030 or 92601 (dependant on VR or Non-VR GP) will be prompted at the finalise visit screen.
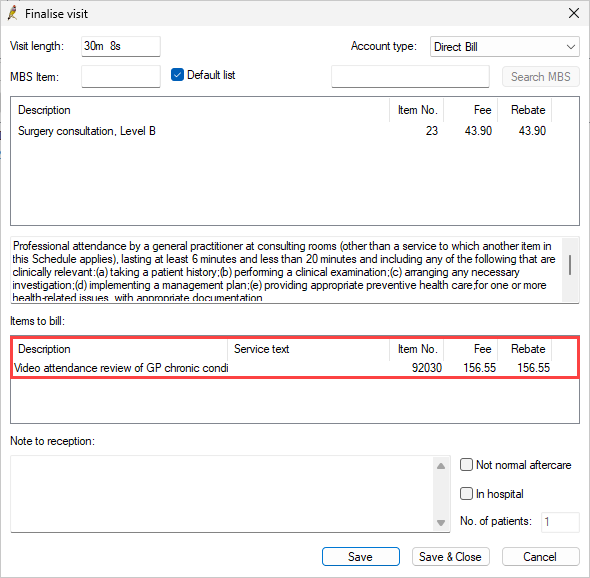
If the appointment type is GP Chronic Condition Management Plan review and the visit type is telephone or telehealth, then review item 92030 or 92601 (dependant on VR or Non-VR GP) will be prompted at the finalise visit screen.
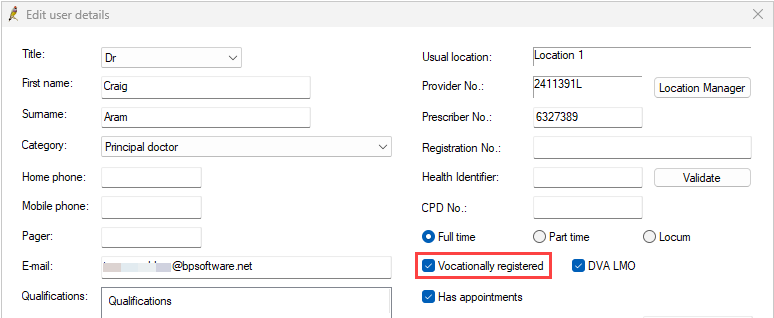
How is Vocationally Registered (VR) and Non-Vocationally Registered (Non-VR) recorded?
VR and Non-VR suggestions are based on the Vocationally registered checkbox on a users profile from Setup > Users > Select User > Edit user details.
Information correct at time of publishing (18 November 2025).