This article includes the questions asked by Bp Premier users during the Spectra SP1 R3 Masterclass sessions delivered by Best Practice Software from September 25th to October 23rd, 2025.
An eLearning module has also been made available covering the Spectra SP1R3 Masterclass content: Bp Premier SP1 Revision 3 eLearning.
Spectra SP1 Revision 3 was released on 30 September 2025, and can be downloaded from the Best Practice website.
All Third Party Integrations and Partners will be making changes to the way they connect to your Bp Premier database, using Halo Connect, by 31st December, 2025. In Spectra SP1 R3, we’ve made important improvements to how third-party integrations are managed in Bp Premier. These enhancements are designed to strengthen data security, improve transparency, and make it easier for your practice to control access to your data.
Standalone Integration Management Window
The Setup Third Party Integrations window has been transitioned to a standalone utility. This change allows practices to manage third-party integrations more efficiently and with greater visibility.
Introduction of Secure Pairing Codes for Bp Partners
To support secure data access, most third-party integrations will now require a Pairing Code to be enabled. When a Bp Partner requires a pairing code, a prompt will appear, allowing a secure code to be generated. Pairing codes are:
- Automatically generated in a secure format
- Unique to your practice
- Visible and manageable through the Setup Third-Party Integrations screen.
Existing integrations that do not require pairing codes will continue to function without interruption.
Improved Integration Controls
The Setup third party integrations screen now includes enhanced prompts and safeguards when enabling or disabling partners:
- Confirmation prompts are displayed before applying changes
- Disabling a partner immediately revokes access and updates system permissions
- Existing pairing codes can be manually closed or regenerated when required.
These updates provide practices with improved visibility and tighter control over third-party data access.
Learn more about the Third-Party Integration changes.
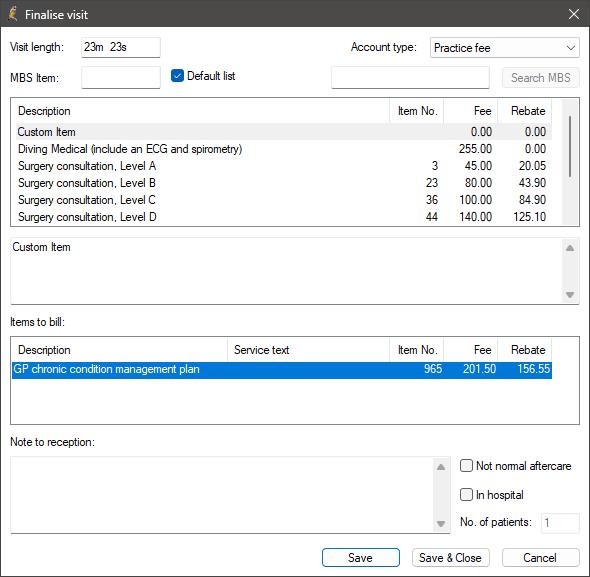
As part of the ongoing support for the Chronic Condition Management (CCM) changes introduced on 1 July 2025, Bp Premier has introduced new claiming logic to improve the handling of relevant MBS item numbers across the finalist visit and invoicing workflows.
In Spectra SP1 Revision 3, Bp Premier will now suggest appropriate item numbers when a user finalises a visit involving the preparation or review of a chronic condition care plan. Bp Premier will determine the correct item based on provider type (VR or Non-VR) and visit mode (face-to-face or telehealth):
Vocationally Registered (VR) GPs:
- Face-to-face: 965 (creation), 967 (review)
- Telehealth: 92029 (creation), 92030 (review)
Non-Vocationally Registered (Non-VR) GPs:
- Face-to-face: 392 (creation), 393 (review)
- Telehealth: 92060 (creation), 92061 (review)
The appropriate MBS item number will be displayed in the item picker based on these criteria.
In Spectra SP1 Revision 3, items of Correspondence can be emailed directly to patients as a PDF file attachment, secured with a PIN, from the Correspondence In screen within the Patient Record.
The document and image file formats listed below can be emailed directly from Patient Record > Correspondence In:
- Documents: PDF, RTF, DOC, DOCX, HTML and TXT
- Images: JPG , JPEG, TIF, PNG, GIF, BMP, TIFF and MTIF.
An Action will be created in Today's notes to show that the Email has been sent, and a Contact Note will be generated for all items of Correspondence sent via Email.
The Australian Government is making changes to the Better Access initiative from 1 November, 2025, to respond to the Better Access program evaluation.
With the removal of the Review and Consultation MBS items for Mental Health Treatment Plans in favour of the time-based items for Preparation, GP’s will have more flexibility to determine the appropriate amount of time needed with a patient based on their individual needs and circumstances to treat the patient.
The following Review and Consultation items will be removed from Bp Premier. The Preparation item numbers will remain and are to be billed for the review and consultation related to a Mental Health Treatment Plan from November 1st going forward. There are no new item numbers being introduced.
|
Review (Removed) |
Consultation (Removed) |
Preparation (Remains) |
|---|---|---|
|
2712 |
2713 |
2700 |
|
92114 |
92115 |
2701 |
|
92126 |
92127 |
2715 |
|
277 |
279 |
2717 |
|
92120 |
92121 |
|
|
92132 |
92133 |
Learn more from the MHTP article.
From November 1 2025, as part of the new eligibility program, changes will be made to bulk billed long-acting reversible contraceptive services (LARCs). These changes include:
- Increasing fees for the existing LARC insertion and removal items (35503, 35506, 14206, 30062)
- Introduction of new items for Nurse Practitioners for insertion and removal (82201, 82202, 82203)
-
Introduction of new loading items that will provide 40% of the fee of the relevant LARC administration item when bulk billed:
- 35501 for GPs and Specialists
- 82204 for Nurse Practitioners.
For the loading item to be payable, the patient cannot be charged any out-of-pocket costs for any MBS items claimed in the LARC insertion or removal appointment, including any co-claimed items relating to provision of the LARC service.
How to bill a loading item
-
From the Finalise Visit screen in the patient record, add the LARC insertion or removal item once completed (35503, 35506, 14206, 30062 or 82201, 82202, 82203 for Nurse Practitioners)
-
Add the new co-claim item (35501 for GPs and Specialists or 82204 for Nurse Practitioners)
-
The new loading item will be inserted above the co-claimed item and will derive a fee amount based on the percentage, in this case, 40%.
Learn more from the complete article.
Information correct at time of publishing (29 September 2025).